Readmission Methodology - Reason for Readmission (Total Readmissions) - Non Risk-Adjusted
Analysis
This methodology applies to the Facility Reason for Readmission (Total Readmissions) Analysis. With this methodology and analysis, you can:
- Define the number of days used to calculate the readmission rate (at the Readmission Days required prompt).
- Identify readmitted cases stratified by diagnoses or other selected characteristics.
Overview
This section provides an overview of the Reason for Readmission (Total Readmissions) Analysis.
- Interval: You define the interval at the Readmission Days prompt (0–365 days can be selected). 30 days is the default.
- All-Cause: Readmissions are for patients readmitted with any diagnosis.
- Patient Type: Readmissions include all inpatient Patient Types by default. You can choose to restrict the analysis to the Inpatient Patient Type at the Readmission Details prompt.
- Readmission Rate: The Readmission Rate is represented by the Readmission Rate value on the analysis.
- Same-Day Readmissions: Same-day readmissions are included by default.
- Risk Method: This analysis is not risk-adjusted.
Readmission Rate
The readmission rate calculation is as follows:
Numerator Readmitted cases to the same facility for a selected population*
Denominator Total cases included in a selected population. Each denominator case can have only one readmission
*The numerator includes same-day readmissions unless they are excluded in the Numerator Selections prompt.
Denominator Exclusions
The denominator exclusions match the discharge status outcome case exclusions from the Risk-Adjusted 30-Day Readmission Analysis.
The following patients are excluded from the denominator:
|
Code |
Description |
|---|---|
|
02 |
Discharged/Transferred to Other Facility |
|
05 |
Discharged/Transferred to Cancer Center or Children's Hospital |
|
07 |
Left Against Medical Advice or Discontinued Care |
|
20 |
Expired |
|
40 |
Expired at Home (For Medicare and Tricare claims for Hospice) |
|
41 |
Expired in Medical Facility |
|
42 |
Expired, Place Unknown (For Hospice) |
|
43 |
Discharged/Transferred to Federal Hospital |
|
66 |
Discharged/Transferred to a Critical Access Hospital (CAH) |
|
82 |
Discharged/Transferred to a short term general hospital for inpatient care with a planned acute care hospital inpatient readmission (effective 10/1/2013 discharges) |
|
85 |
Discharged/Transferred to a Designated Cancer Center or Children's Hospital with a planned acute care hospital inpatient readmission (effective 10/1/2013 discharges) |
|
88 |
Discharged/Transferred to a federal health care facility with a planned acute care hospital inpatient readmission (effective 10/1/2013 discharges) |
|
94 |
Discharged/Transferred to a Critical Access Hospital (CAH) with a planned acute care hospital inpatient readmission (effective 10/1/2013 discharges) |
Readmission Days Prompt
In the Readmission Days prompt on the Select Population tab, you define the readmission interval, which identifies the readmitted cases to include in the analysis. “30 Days” is entered by default.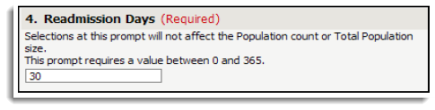
The system looks forward from the Discharge Date for each patient included in the denominator and identifies each readmitted case that is less than or equal to the Readmission Days selected. The system identifies readmitted cases beyond the selected population’s timeframe up to the Readmission Days selected.
Population Selection and Patient Types
All prompt selections, except Patient Type, determine the population for which the system will report readmissions (numerator cases).
The selected Patient Type applies to both the denominator and numerator cases.
- If more than one Patient Type is selected (such as Inpatient (08), Rehabilitation (23), Psychiatric (24), and Chemical Dependency (26)), the denominator and numerator cases could have any of the values selected.
- If one Patient Type is selected (such as Inpatient (08)), the selected value applies to both denominator and numerator cases.
Only the Patient Type prompt may be used to exclude certain patient types from both the population (denominator cases) and readmissions (numerator cases).
Index Admissions and Readmissions Comparison
This section uses an example to help explain the relationship between index admissions and readmissions.
In the following example, June 2010 is selected at the time prompt.
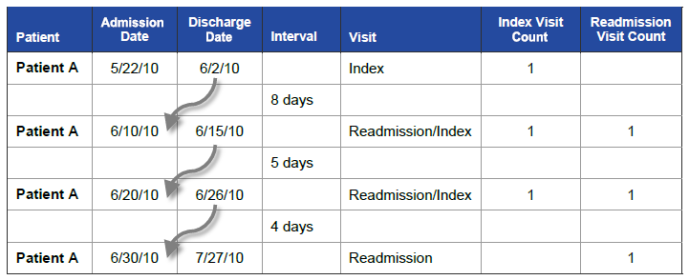
Two visits count as both an index admission and a readmission.
- Only admissions with Discharge Dates in June 2010 are included in the population, because the index visit is evaluated for readmission on the first subsequent inpatient admission that occurs within 30 days of index discharge.
- If the last readmission is outside the timeframe, it will be counted as a readmission.
Risk-Adjusted 30-Day Readmission Analysis
- If the interval between the Discharge Date and the subsequent Admission Date is within 30 days, the next Acute Inpatient unplanned admission counts as a readmission.
- The data is based on the index visits included in the analysis. In the example above, only the first three patient visits would be included in the patient population for the analysis.
Reason for Readmission (Total Readmissions) Analysis
- If the interval between the last discharge date and the next admission is within the number of days defined at the Readmission Days prompt, the next admission counts as a readmission.
- The data is based on the readmission visits included in the analysis. In the example above, only the last three patient visits would be included in the patient population for the analysis, because they occur within the selected “Readmission Days” of the discharge dates for the corresponding index admissions.
Reason for Readmission (Planned vs Unplanned) Analysis
- If the interval between the last discharge date and the next admission is within the number of days defined at the Readmission Days prompts, the next Acute Inpatient admission counts as a readmission.
- The data is based on the readmission visits included in the analysis. In the example above, only the last three patient visits would be included in the patient population for the analysis, because they occur within the selected “Readmission Days” of the discharge dates for the corresponding index admissions.