January 15, 2024
Expand any topic listed below to see the details included in this release.
QualityAdvisor is now updated with AHRQ version 2023 for Standard Analyses and Custom Query for IQI and PSI (Facility & Peer). This version represents CMS FY2023. Additionally, this version includes COVID-19 discharges since AHRQ is able to provide risk- adjustment for COVID-19 patients (Present on Admission) with this version.
-
AHRQ v2023 supports all retrospective coding, and new coding effective with CMS FY 2023 (10/1/22 and forward)
-
The version supports coding up to 9/30/2023
-
A v2022 report option will be maintained for all total inpatient PSI, IQI, and PSI-90 report versions
Notes:
- AHRQ v2023 is now the default prompt selection for AHRQ PSI, IQI, and PSI-90 reporting for the analyses mentioned above
-
AHRQ v2023 is retroactive to 7/1/2018 in QualityAdvisor, and includes CMS supported coding through 9/30/2023
-
Premier Statistics provided are for v2023 and are based on 10/1/2022 - 9/30/2023
-
Risk-adjustment was provided by AHRQ within v2023 by using the Health Care Cost and Utilization Project (HCUP) reference population
- As with previous AHRQ versions, Premier will pass the first 35 diagnosis and 30 procedure codes through the software
- Individual PSI Technical Specification Updates include CMS annual coding updates (for ICD, MS-DRG and MDC), and POA exempt code updates
AHRQ v2023 is now available on the following analyses:
- PSI – Standard Analysis, and Custom Query for Facility and Peer
- IQI – Standard Analysis, and Custom Query for Facility and Peer
- PSI-90 Total Inpatient – Standard Analysis
Note: AHRQ v2021 is retired for PSI and PSI-90 Total Inpatient, and AHRQ v2019 is retired for IQI
PSI Specific Changes:
PSI-08 expansion
-
In v2023, the PSI-08 numerator is expanded from "In Hospital Fall with Hip Fracture Rate" to "In-Hospital-Fall-Associated Fracture rate" and is made up of two components:
PSI-08 Hip (only hip fractures)
PSI-08 Other (broader range of fractures associated with an in-hospital fall)
-
The risk-adjusted results are provided for the overall PSI-08
-
Components are mutually exclusive, and hip fractures take priority. If both a hip fracture and a non-hip fracture occur, discharges are assigned to the hip fracture component. If only a non-hip fracture occurs, discharges are assigned to the other fracture component
PSI-06- denominator exclusion
-
Replaced denominator exclusion of iatrogenic pneumothorax diagnosis codes with exclusion of non-traumatic pneumothorax diagnosis codes
PSI-12- denominator exclusion
-
Added denominator exclusion for any secondary diagnosis of heparin-induced thrombocytopenia (HIT)
PSI-15- numerator updates
-
Revised numerator criteria requiring anatomic site-specific procedure code lists to match repair procedures with same site accidental puncture or laceration diagnosis
PSI Analyses Notes:
-
Premier Statistics for v2023 are based on 10/1/2022 - 9/30/2023
-
All of the same numerator and count measures based on v2023 are also included within the Patient Qualifications prompt
-
V2021 has been retired, v2023 has been added as the new report default and caution messages are updated to reflect v2022 software supported timeframe
PSI-90 Total Inpatient Analysis Notes:
- The same v2023 software used for the PSI – Standard Analysis is used for this PSI-90 Total Inpatient report and includes a PSI-90 Composite. The v2023 Technical Specifications can be used as reference documentation for the PSI individual measures
- This is an all payer version, all inpatient, flexible timeframe report
IQI Specific Changes:
Procedure Day Requirements
-
In v2023, the IQI module requires procedure date to assign AHRQ Clinical Classification Refined (CCSR) for ICD-10_PCS Procedures which impacts the following procedure-based indicators (IQI 08, 09, 11, 12, 30, 31)
-
Missing or incomplete procedure date information will impact risk-adjusted rates for these indicators
IQI-15
-
Replaced a risk category for non-ST-elevation myocardial infarction (non-STEMI) with a risk category for ST-elevation myocardial infarction (STEMI) based on all diagnosis code positions for potential feature selection to IQI 15 – Acute Myocardial Infarction (AMI) Mortality Rate
With this January release, we have added Standard Secondary Payer information to QualityAdvisor reporting as requested by our members. The Secondary Payer is a data element that is already submitted through the discharge file, but until now was not displayed in QualityAdvisor. The intention of adding this information is to promote better understanding of patient's dual eligibility.
The Secondary Payer attribute is added to the Standard Payers optional prompt on the Select Population tab for:
-
Standard Analyses, Custom Query, Outpatient View
-
Facility and Peer reporting
-
CareScience and 3M risk models
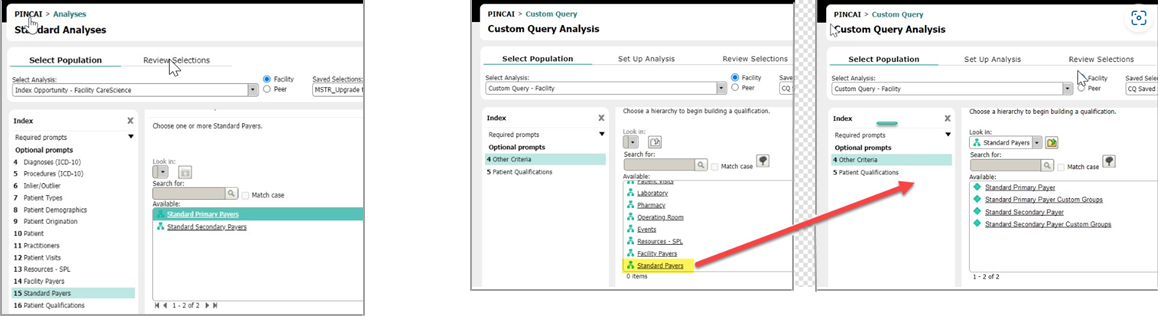
Custom Groups will enable you to easily identify dual eligible patients by filtering your reporting population by a combination of Standard Primary and Standard Secondary Payers. If you create a Standard Payer Custom Group with Medicare and Medicaid criteria selections and then utilize it to filter your reporting population, patients with Medicare or Medicaid as their Standard Primary Payer AND Medicare or Medicaid as their Standard Secondary Payer will return on your analysis.
Notes:
-
Secondary Payer is not a required data element, but can be submitted for both inpatients and outpatients. (Primary Payer remains a required data element)
-
Standard Payer options are the same for both Primary and Secondary Payers
-
Secondary payer is defined as the payer value submitted in the #2 ranked position. Users will only be able to report on one secondary payer
-
The existing Standard Payer attribute description is updated to now read as Standard Primary Payer throughout QualityAdvisor. You will now see both Standard Primary Payer and Standard Secondary Payer options
-
The Risk Calculator is updated to display Standard Primary Payer. Secondary Payer is not added since it is not included in the CareScience risk model
-
You must manually update Saved Analyses, Saved Selections, Favorites, and Custom Groups if you wish to include Secondary Payers
-
Secondary Payer has not been added to the Facility Payer prompt so when drilling to Facility Payer from Standard Secondary Payer, the analysis will return the Facility Primary Payer that has been submitted
We have updated THA/TKA Complication measure (observed) methodology within QualityAdvisor to use the new FY24 THA/TKA Focused Population and new THA/TKA benchmark values.
Note: With this year's update, there is a VBP version and IQR version. QualityAdvisor uses the IQR version.
Per the Yale documentation, the following measure changes for 2023 which pertain specifically to the observed values are as follows:
-
Addition of 26 ICD-10 codes that define the 'Mechanical Complications" outcome, as finalized in the FY2023 IPPS Rule
The addition of the 26 codes applies only to the THA/TKA complication measure as included in the Hospital Inpatient Quality Reporting Program (FY 2024 payment determination) and publicly reported on Care Compare. It does not apply to the THA/TKA complication measure as included in the FY 2024 Hospital VBP Program
The addition of these clinically relevant codes contributed to an increase in the national observed complication rate of 0.8%
-
Addition of 6 procedure codes to the “Periprosthetic Joint Infection/Wound Infection and Other Wound Complications” and “‘Surgical Site Bleeding and Other Surgical Site Complications’ code lists
-
Changes to Cohort Exclusions include the addition of ICD-10-CM codes to the list of codes that identify a THA/TKA procedure as non-elective or non-primary and disqualify the admission from THA/TKA cohort inclusion
Added 2 codes to the list defining Fracture (Periprosthetic)
Added 2 codes to the list defining Mechanical Complications
CMS has published an updated version of the ICD-10 CMS Hospital Acquired Conditions (HAC) for CMS FY2024. With this January release, the updated ICD-10 HACs, effective starting with October 1, 2023 discharges, have been implemented in the QualityAdvisor application.
HAC Diagnoses
-
No HAC diagnoses added
-
No HAC diagnosis deleted
HAC Procedures
-
54 HAC procedures added to HAC 13 — SURGICAL SITE INFECTION (SSI) FOLLOWING CARDIAC IMPLANTABLE ELECTRONIC DEVICE (CIED) PROCEDURES (effective with 10/1/2023 discharges)
-
No HAC procedures deleted
Additional Notes:
-
Patients discharged from October 1, 2023 and forward group to the FY2024 CMS HAC list
-
Analyses impacted by this change include: Complications Comparison (Facility and Peer), Complications Distribution (ICD-10 for both Facility and Peer), and CMS Hospital Acquired Conditions (Facility)
-
Reports run for time periods that cross over multiple fiscal years will see a mix of the different CMS HAC versions (i.e., 7/1/2018, 10/1/2018, 10/1/2019, 10/1/2020, 10/1/2021, 10/1/2022, and/or 10/1/2023)
-
All Fiscal Year HAC lists are available in Chapter 8 of the Methodologies Guide
This January release includes the FY2024 Potential Inpatient Complications (PIC) list defined by Premier. A summary of the updates is listed below, and the detailed PIC list is available in the ICD-10 Knowledge Center as well as in Chapter 8 of the Methodologies Guide.
PIC Diagnoses
-
11 PIC diagnoses are added (effective with 10/1/2023 discharges):
1 PIC diagnosis added for 101- Sepsis
1 PIC diagnosis added for 109- Other Infections
3 PIC diagnoses added for 602- Encephalopathy
1 PIC diagnosis added for 901- Acute Myocardial Infarction
2 PIC diagnoses added for 902- Complications of Acute myocardial infarction (AMI)
2 PIC diagnoses added for 1001- Pneumonia
1 PIC diagnosis added for 1801- Coma
-
No diagnoses expire
PIC Procedures
-
3 PIC procedures are added for 1010- Acute Respiratory Failure
-
No PIC procedures are expired with this release
Additional Notes
- Analyses impacted by this change include: Complications Comparison (Facility and Peer) and Complications Distribution (ICD-10 for both Facility and Peer)
-
Patients discharged from October 1, 2023 and forward will group to the FY2024 PIC list
- Reports run for time periods that cross over multiple fiscal years will see a mix of the different PIC fiscal year versions (i.e., 7/1/2018, 10/1/2018, 10/1/2019, 10/1/2020, 10/1/2021, 10/1/2022, and/or 10/1/2023)
The annual perinatal measure update includes a measure enhancement and new ICD10 codes which became effective on 10/1/2023. The following updates are specific to two Obstetrics measures within Custom Query. Additional details can be referenced in the updated Codes and References documentation within the Perinatal Quality Dashboard Help, which also includes updates specific to PQD.
-
Maternal Sepsis – 1 new code added
-
Uterine Rupture – 3 new codes added
Go to the Archives to see Release Notes for previous releases