July 28, 2025 Release Notes
This is where you can read about new features or enhancements that have been released in the QualityAdvisor application.
Expand any topic listed below to see the details included in this release.
Here is what's new in QualityAdvisor™ as of July 28, 2025:
With this July release, we have added the 2024 version (Version 13.0) of the CMS Hospital-Wide Readmission methodology and Planned Readmission Algorithm to QualityAdvisor's risk-adjusted reporting. The newly added methodology is called the CMS All-Cause Hospital-Wide (HWR) 30-Day Readmission based on Planned Readmission Algorithm (PRA) v4.0 2024. This methodology applies to patient discharges beginning October 1, 2020 and forward.
QualityAdvisor maintains two versions of CMS Readmission methodologies to allow you to choose when to move to the latest methodology. The current versions now include:
-
CMS All-Cause Hospital-Wide 30-Day Readmission (HWR) Methodology Based on PRA v4.0 2024 (discharges October 1, 2020 and forward)
-
CMS All-Cause Hospital-Wide 30-Day Readmission (HWR) Methodology Based on PRA v4.0 2023 (discharges October 1, 2020 and forward)
Note: The CMS All-Cause Hospital-Wide 30-Day Readmission (HWR) Methodology Based on PRA v4.0 2022 is removed with this release.
Summary Overview
The 2024 version of the Hospital-Wide Readmission methodology (HWR PRA v4.0 2024) is very similar to past versions. There are no flowchart or algorithm changes to the HWR methodology itself or the Planned Readmission Algorithm.
The following updates have been made to the HWR measure for Version 13.0 with the intent to maintain the clinical integrity of the algorithm and cohort definitions:
Changes to the planned readmission algorithm:
-
Potentially planned procedures:
-
Added one ICD-10-PCS code (associated with AHRQ CCS procedure category 49) to the singular ICD-10-PCS code list
-
-
Acute diagnoses
-
Added ICD-10-CM codes (associated with AHRQ CCS diagnosis categories 97, 101, 106, 115, 233, 238, 244, and 662) to the singular ICD-10-CM code lists
-
-
The following COVID-19 modifications that were introduced with version 2022 will continue for this version of reporting:
-
A ‘History of COVID-19’ risk variable is incorporated into the risk-adjustment model
-
COVID-19 index admissions are excluded from the cohorts. COVID-19 index admissions are defined by a principal diagnosis code of COVID-19 or a secondary diagnosis code of COVID-19 coded as POA on the index admission claim
-
COVID-19 readmissions are not eligible for the readmission outcome and are excluded. COVID-19 readmissions are defined by a principal diagnosis code of COVID-19 or a secondary diagnosis code of COVID-19 coded as POA on the readmission claim
-
Notes
-
A new prompt option for the HWR PRA v4.0 2024 methodology has been added to all relevant analyses
-
All relevant analyses have been updated to include Readmission metrics based on the new HWR PRA v4.0 2024 methodology
Additional information is available in the Inpatient Methodologies Guide Chapter 7 - Readmissions >All-Cause Hospital-Wide 30-Day Readmission Methodology based on PRA v4.0 2024.
Updated population tables are available in PRA Version 4.0 2024 - Overview and Population Tables.
This July release includes a significant change to system level readmissions. Until now, system level readmissions did not exclude same-day transfers between hospitals of the same health system unless they meet certain exclusion criteria (e.g., discharge status), resulting in the transfers being recorded as two separate visits, with the second being counted as a readmission.
Now, same-day transfers within the same health system are recognized as one visit instead of two. The visit that is used as the index and eligible for a readmission is the second visit instead of the first.
-
This update will be applied to both HWR PRA v4.0 2023 and HWR PRA v4.0 2024 at the system level only. There will be no change to entity level results
-
The measure considers multiple hospitalizations that result from hospital-to-hospital transfers as a single acute episode of care
-
Admissions to a hospital within one day of discharge from another hospital are considered transfers regardless of whether the first institution indicates intent to transfer the patient in the discharge disposition code or whether the second inpatient admission is for the same condition
-
For patients transferred from one short-term acute care hospital to another, only the last admission in the series of transfers is eligible for inclusion in the cohort. The previous admissions are not included
We have completed our annual calibration updates, which affect all of the CareScience and 3M™ Risk-Adjusted Outcomes: Cost, Charges, Length of Stay (LOS), Readmissions, Complications, and Mortality.
With the 2025 Calibration update, data is re-scored for patient discharges from 10/1/2024 and forward for both CSA Inpatient and Outpatient Outcomes.
We have also updated to the APR DRG Grouper v42.0 for patient discharges beginning 10/1/2024 and forward.
-
Eight quarters of data, inclusive of 4Q2022-3Q2024 data, is used to calculate the 2025 calibration updates for both Inpatients and Outpatients
-
The 2025 scaling factors are applied to all CareScience outcomes for patient discharges beginning 10/1/2024 and forward, except for the Charge outcome (only Standard Practice expected values calculated for this outcome) and new HWR PRA v4.0 2024 outcome
-
The 2025 CSA Outpatient calibrations data is re-scored from 10/1/2024 and forward for the following outcomes:
-
Same Day Surgery Returns to ED (within 1, 3, 7, 30 days) – 4 outcomes
-
Observation Returns to ED (within 1, 3, 7, 30 days) – 4 outcomes
-
ED Returns to ED (within 1, 3, 7, 30 days) – 4 outcomes
-
ED Returns and Admitted as Acute Inpatient (within 4-7 and 30 days) – 2 outcomes
-
2025 CSA ICU Calibrations
ICU Risk Adjusted Metrics were added to QualityAdvisor in August 2024.
With this 2025 CSA ICU calibrations update, data is re-scored from 10/1/2024 and forward for ICU patients only and the following outcomes:
-
Mortality in ICU
-
Length of Stay in ICU
-
ICU Patient Ventilator Days
-
Return to ICU
-
Returns to ICU within 48 hours
-
ICU Patient Mortality
-
ICU Patient Length of Stay
As is the case with the CSA Inpatient calibrations, eight quarters of data, inclusive of 4Q 2022 - 3Q 2024 data, is used to calculate the 2025 ICU calibration updates.
Reminders:
-
Some of the above outcomes are calculated at the episode level for each patient and others are calculated at the patient level for the entire visit
-
There is no CSA-ICU 2024 model year because the ICU Outcomes Comparison Analysis was newly released using the CSA-ICU 2023 model. Patients prior to 10/1/24 will continue to return results based on the CSA-ICU 2023 model year
Notes
-
Please review the Annual Calibration Updates for 2024 for detailed information
-
A Frequently Asked Questions document all about CSA Risk Adjustment Methodology is available in Chapter 3 of the Inpatient Methodologies Guide
- As a reminder, if a patient qualifies as an outcome case for length of stay, charges, or cost, there is logic used in the CareScience model to determine if the patient's calculated risk falls within the allowable range (trim point values or CSA outlier logic). Every year the minimum and maximum values are updated with new ranges to account for changes in care practice
-
The Data Vintage Factor Adjusted Outcome Analysis Facility and Peer reports are updated to account for both the annual 2025 calibration updates, and the CareScience Analytics model enhancements
-
Select Practice is not currently available for CSA ICU or CSA OP risk-adjustment and will not be added with this year’s calibration release
Premier has refreshed the outlier minimum and maximum values using calendar year 2023 data. Prior to this release, the boundary values were based on calendar year 2022 data.
The impact to the number of outliers in the database is minimal, shifting from 9.9% of inpatients currently as outliers to 9.7% of inpatients as outliers as a result of the change.
Refer to the Outlier Prompt Methodology for more information.
Notes
- The Outlier updates will also be available in CPM Hospital and Quality Console once the profile definitions and dashboards have been reprocessed with a data release.
The Facility Profiling Analysis now reflects metrics based on data from CMS FY2024 (October 1, 2023 to September 30, 2024).
The DVF Adjusted Outcome Analysis provides an automated solution for users who would like to stabilize trended reporting across one or more calibration cycles. This analysis allows you to analyze trends from year to year while holding the benchmark at the fixed baseline. All CSA 2025 Model Year changes are incorporated into each version of the DVF Adjusted Outcome Analyses (Facility & Peer, CareScience & 3M).
Notes
-
The new HWR PRA v4.0 2024 Readmission methodology will not be added to the report this year, since there is no DVF needed, and that outcome is available within other reporting options
-
The HWR PRA v4.0 2023 Readmission methodology is added to the report this year
-
The HWR PRA v4.0 2022 Readmission methodology is retired
The Disease Strata by Outcome analysis was introduced to QualityAdvisor in October 2022, following the CSA 2022 move to CCSR disease strata. With this July 2025 release, the analysis is updated with the new CSA 2025 calibrations.
Notes
-
The CSA 2025 version replaces the CSA 2024 version for this analysis
-
There are 3 new CCSR categories with CSA 2025:
-
CCSR_DX_NEO075- Leukemia in remission
-
CCSR_DX_NEO078- Myeloma in remission
-
CCSR_DX_SYM018- Prediabetes
-
-
Readmissions metrics now include both HWR Methodology Based on PRA v4.0 2024 and PRA v4 2023
-
Readmission metrics based on HWR PRA v4 2022 are removed
With this release, we updated the Risk Calculator to factor in all relevant aspects of this July 2025 release, including:
-
All CSA 2025 Risk Model year updates
-
All calibration updates
-
The addition of the new All-Cause HWR PRA v.4.0 2024 Readmission methodology
Notes
-
A new tab has been added for the new All-Cause HWR PRA v.4.0 2024 Readmission methodology
-
HWR PRA v4.0 2022 Readmission methodology has been retired from the Risk Calculator
-
With the addition of the new CSA 2025 model year, the oldest model year (CSA 2022) has been rolled off of the calculator
With this release, Premier has completed the annual archiving of data from the QualityAdvisor database. All FY2020 data is removed.
Notes
-
2020 remains as a reporting prompt under "Year," however analyses will only return data between Oct 1, 2020 - Dec 31, 2020
-
At least 5 years of data is maintained within QualityAdvisor to balance an adequate reporting time frame and optimum database performance
-
The PSI-90 for CMS HACRP 2024 V13 is retained and remains on Time Prompt and Program Year Parameters options
The following Perinatal measure updates are implemented for Custom Query and the Perinatal Quality Dashboard (Facility and Peer for 3M, CareScience, and Analytical Views), effective for April 1, 2025 discharges and forward:
-
1 procedure code is added to induction of labor impacting all induction of labor measures
-
0U7C7DJ - Dilation of cervix with intraluminal device, temporary, via natural or artificial opening
-
-
8 codes removed from the sickle cell crisis category, impacting the maternal hemorrhage measures
-
D57.03 - HB-SS DISEASE WITH CEREBRAL VASCULAR INVOLVEMENT
-
D57.09 - HB-SS DISEASE WITH CRISIS WITH OTHER SPECIFIED COMPLICATION
-
D57.213 - SICKLE-CELL/HB-C DISEASE WITH CEREBRAL VASCULAR INVOLVEMENT
-
D57.218 - SICKLE-CELL/HB-C DISEASE WITH CRISIS WITH OTHER SPECIFIED COMPLICATION
-
D57.413 - SICKLE-CELL THALASSEMIA, UNSPECIFIED, WITH CEREBRAL VASCULAR INVOLVEMENT
-
D57.418 - SICKLE-CELL THALASSEMIA, UNSPECIFIED, WITH CRISIS WITH OTHER SPECIFIED COMPLICATION
-
D57.813 - OTHER SICKLE-CELL DISORDERS WITH CEREBRAL VASCULAR INVOLVEMENT
-
D57.818 - OTHER SICKLE-CELL DISORDERS WITH CRISIS WITH OTHER SPECIFIED COMPLICATION
-
-
6 codes are removed from SMM impacting all SMM measures
-
I63.02 - CEREBRAL INFARCTION DUE TO THROMBOSIS OF BASILAR ARTERY
-
I63.031 - CEREBRAL INFARCTION DUE TO THROMBOSIS OF RIGHT CAROTID ARTERY
-
I63.032 - CEREBRAL INFARCTION DUE TO THROMBOSIS OF LEFT CAROTID ARTERY
-
I63.033 - CEREBRAL INFARCTION DUE TO THROMBOSIS OF BILATERAL CAROTID ARTERIES
-
I63.039 - CEREBRAL INFARCTION DUE TO THROMBOSIS OF UNSPECIFIED CAROTID ARTERY
-
I63.09 - CEREBRAL INFARCTION DUE TO THROMBOSIS OF OTHER PRECEREBRAL ARTERY
-
Notes:
Perinatal measures do not have versioning. This means:
-
When new or additional codes are added to a measure, the measure volumes will update automatically as soon as members begin using those codes
-
Volumes may decrease if the new codes are designated as exclusions within the measure
-
If CMS retires certain codes, those codes are no longer being used going forward. However, they will still be included in the measure for discharge dates during which they were valid.
-
When codes are deleted from a measure, they are removed entirely. This affects both future and historical volumes
The 100 Top Hospital Peer Group option was added to QualityAdvisor in April 2024. At that time, the only peer list available was the 2023 Top Hospital winners. With this July 2025 release, we are adding both the 2024 and 2025 Top Hospital winners as separate peer groups. You will now see all three peer group options in the Premier Initiatives parent folder.
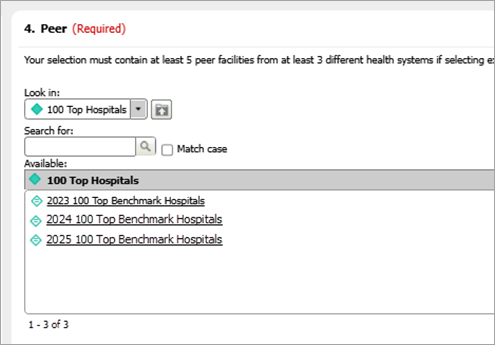
The 100 Top Hospital peer group includes the Quality Enterprise and QualityAdvisor members that receive the 100 Top Hospitals award at Premier's annual Breakthroughs conference each summer.
Notes:
-
This is a static list and hospitals only populate if they are an active QualityAdvisor subscriber that has published data to the comparative warehouse
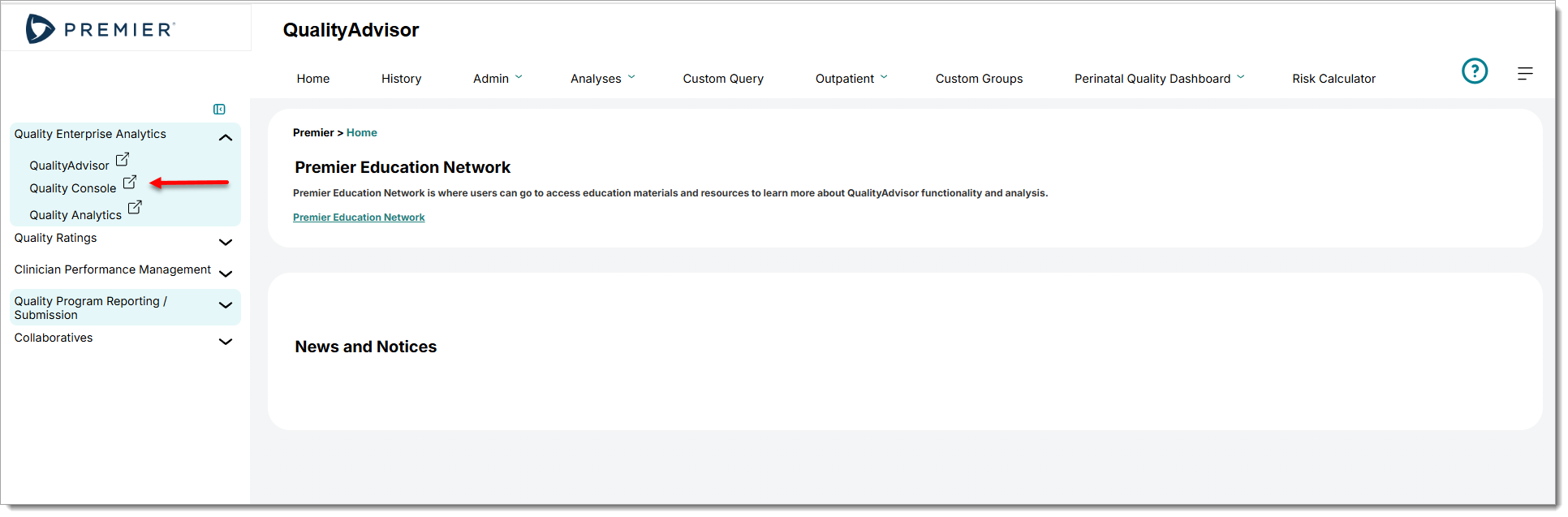
This July 2025 release includes a refresh to the overall look and feel for Quality Enterprise applications. Other than the new look, you will notice that the link to the Quality Console application is now located in the left navigation panel instead of its original location in the top tool bar.
Go to the Archives to see Release Notes for previous releases